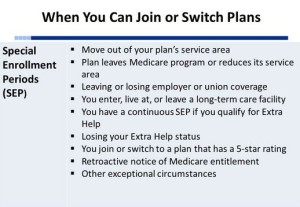
UPDATED Feb. 7, 2019. Typically, you may join, change or leave a Medicare Advantage plan or Part D plan in one of three enrollment periods: Initial Enrollment Period when you first qualify for Medicare, Medicare Open Enrollment Period (Oct. 15-Dec. 7), and Medicare Advantage Open Enrollment Period (Jan.1 – Mar. 31). Outside of these three periods, you may change your coverage only during Special Enrollment Periods (SEPs), if you are qualified.
Below we provide a list of major (but not all!) SEPs – the required conditions, how long the SEP lasts and when the coverage begins.
1. Special Enrollment Periods (SEPs) – Drop employer/union coverage
- Condition: You are disenrolled from an employer or union group health plan (including COBRA coverage) to enroll in a Medicare Advantage or Part D
- Your SEP lasts: Two months after the month your coverage through the group plan ends
- Coverage begins: The first day of the month after you submit an application, or up to 2 months after your SEP ends (if requested)
2a. Special Enrollment Periods (SEPs) – Eligible for Medicaid
- Condition: You have Medicaid
- Your SEP lasts: The first month you become eligible for Medicaid. As long as you have Medicaid, you can switch health or drug plans once a month.
- Coverage begins: The first day of the month after you submit an application to the Medicare Advantage plan or Part D plan
2b. Special Enrollment Periods (SEPs) – Lost Medicaid
- Condition: You lose your full Medicaid benefits
- Your SEP lasts: You have one SEP to switch your Medicare Advantage or Part D plan. It begins the month you are notified that you will lose Medicaid and continues for two months after.
- Coverage begins: The first day of the month after you submit an application
3a. Special Enrollment Periods (SEPs) – Eligible for Extra Help
- Condition: You become eligible for Extra Help
- Your SEP lasts: You may join, switch or disenroll from Medicare Advantage plans with drug coverage (or stand alone Prescription Drug plan) beginning the month you become eligible for Extra Help. As long as you have Extra Help, you can switch plans once a quarter.
- Coverage begins: The first day of the month after you submit an application.
3b. Special Enrollment Periods (SEPs) – Lost Extra Help
- Condition: You lost the Extra Help
- Your SEP lasts: You have one-time SEP to disenroll from or switch your Medicare Advantage plan or Part D plan for two months after you are notified of Losing Extra Help.
- Coverage begins: The first day of the month after you submit an application.
4. Special Enrollment Periods (SEPs) – Permanent Move
- Condition: You move permanently. You have SEP if you move out of the area of your Medicare Advantage / Part D plan. You also have SEP if you plan is in the new coverage area, but more plans are available there.
- Your SEP lasts: If you’ve notified the plan before you move, you SEP starts a month before you move and lasts up to two months after the move. If you’ve notified the plan after the move, you SEP starts the month you tell the plan and lasts two more months thereafter.
- Coverage begins: Any time between the first day of the month you move and up to three months after the plan receives the completed application.
5. Special Enrollment Periods (SEPs) – Disenrollment from your first Medicare Advantage plan
- Condition: You select a Medicare Advantage plan when you first qualify for Medicare around 65 (ICEP).
- Your SEP lasts: You can disenroll from your Medicare Advantage plan at any time during the 12-months after your health plan started and go back to original Medicare with or without a stand-alone Part D plan.
- Coverage begins: Depends upon the situation.
6. Special Enrollment Periods (SEPs) – Enrolled in the qualified SPAP program
- Condition: You are enrolled in a qualified State Pharmaceutical Assistance Program (SPAP)
- Your SEP lasts: You have a SEP to choose once per year, anytime. You may join or change Medicare Advantage / Part D plan. You may not drop Part D coverage.
- Coverage begins: The first day of the month after you submit an application.
US Government Sources
Please give us your feedback!
What do you think about Special Enrollment Periods (SEPs) for Medicare Advantage and Part D? Write your comments.
Contact Us
For help finding the best for YOU Medicare Plan or Individual Health Plan, please contact Liberty Medicare or call us at 877-657-7477.





Comments are closed.